Sarah Pack, Medical University of South Carolina
There are so many universities doing fast development alongside companies pitching in to produce a range of personal protective equipment (PPE), ventilators, respirators, and all the components required – so just a warning, this list is long. Most news items have been shortened and there are links to all the companies and what they are doing so you can reach out and connect to them. Stay healthy and keep us posted on how your business is doing.
Medical University of South Carolina team releases plans for 3D-printed masks
The team has been in contact with the FDA to obtain emergency approval of the device, talking to manufacturers to see if the design can be mass produced.
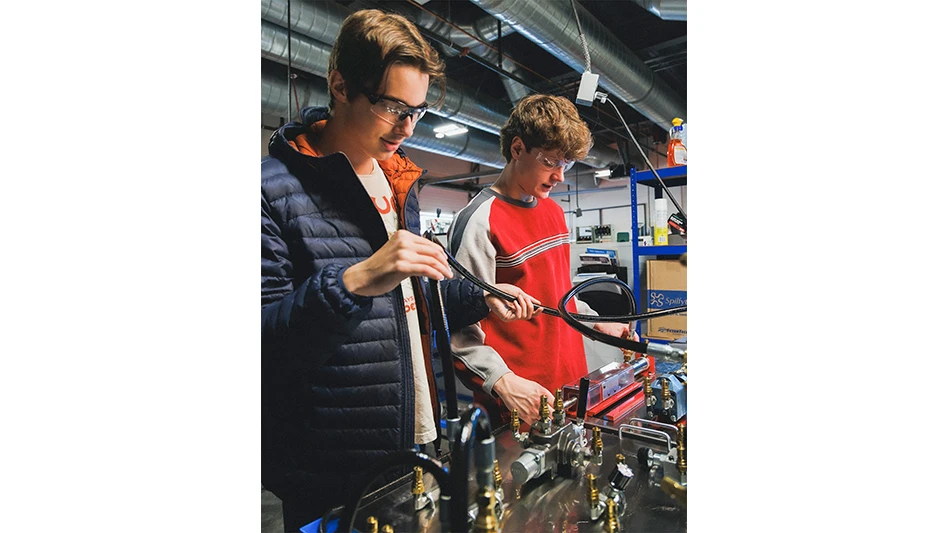
With the threat of a shortage of protective masks looming as the novel coronavirus pandemic grows, Medical University of South Carolina (MUSC) biomedical engineers and tinkerers had an inspired idea: unleash an army of makers from across the U.S. who could make such masks from 3D printers - a technology that, in recent years, has become widely available.
"High schools have a printer capable of making this," said Michael Yost, Ph.D., vice chair of research in the Department of Surgery. "Let's make this so simple that a high schooler could do it, yet effective to protect our people."
In a matter of days, a team came together and developed the Self-Assembly Filter for Emergencies, or SAFE, Cartridge System. The system could be used by medical professionals or by people who just need to go to the grocery store.
The team has been in contact with the U.S. Food and Drug Administration to obtain emergency approval of the device. For now, the device remains investigational and should not be used as a replacement for conventional and approved Personal Protective Equipment.
Yost says the team is talking to manufacturers to see if the design can be mass produced once it has received approval.
The N95 masks that are currently in such short supply are essentially filters molded into mask form. Recreating those masks exactly proved too difficult. So instead, the team created a two-part solution: a 3D printed mask that can be cleaned and reused that will work in tandem with a 3D printed disposable filter cartridge. Alternatively, the filter cartridge could be used with an adapted hospital mask.
Joshua Kim, senior designer and program coordinator in the Department of Surgery Human-Centered Design Program, said he was inspired by the NASA engineers during the Apollo 13 disaster, who quickly devised a makeshift carbon dioxide removal system from materials on hand inside the lunar module, including duct tape and plastic.
"How can we utilize materials that people can get at a local hardware store and repurpose those materials to make protective equipment?" he asked.
The "95" in N95 means these masks filter 95% of particulates of a certain size, he explained. HEPA filters, like those used in air purifiers, filter around 99% of particulates. So he bought a HEPA filter and set about experimenting. Using the same testing that's used on N95 masks, he found that using those filters in the homemade cartridge did work - a positive sign that they were on the right track.
Meanwhile, another group was working on creating the masks. Dentists Walter Renne, D.M.D., and Christian Brenes Vega, D.D.S., regularly use 3D printing. "It's just a part of the job," said Renne, who estimated that 20% of dentists and 90% of dental labs have a 3D printer on hand. They enlisted the help of John Yost, a student and independent contractor who serves as a resource for all things associated with 3D printing on campus.
A team at MUSC developed a DIY protective mask that anyone with a 3D printer can copy.
Initially, they developed different prototypes that would work with different types of filters, including filters used by painters or people dealing with asbestos. They 3D scanned a mask to get the basic shape, then designed modifications so the mask could accommodate the disposable filter cartridge. The filter, noted Brenes Vega, is the most important part. Unfortunately, some people have turned to masks that aren't actually offering protection, he says.
Finally, they needed to solve the problem of releasing air pressure, Kim says. The filters are so effective that when the wearer exhales, the air will go to the area of least resistance to escape - in other words, not through the filter again but by causing the mask to lift slightly off the wearer's face. That exposes the wearer to the outside air and renders the mask worthless, Renne said. In response, the team installed a rubber valve, commonly used in other medical applications, that allows the exhaled air to escape the mask. As soon as the wearer inhales, the valve immediately shuts, Kim says, protecting the wearer.
Kim notes that, for additional sealing and comfort, they added strips of neoprene weatherstripping foam around the edges of the mask. The foam provides a comfortable fit so the wearer's skin isn't touching the plastic mask and ensures it contours to the face as the wearer moves or talks.
With all the parts in place - the 3D printed mask and 3D printed cartridge fitted with a hand-cut HEPA filter and rubber valve - the group began fit-testing.
They took four prototypes to the Emergency Department and tested them on several users. So far, the masks have fit everyone, Yost said, although they want to expand their testing to include more face sizes and shapes.
The team is already printing masks at MUSC, even as they continue to perfect the design.
The biggest obstacle now is the time it takes to create the masks. MUSC's 3D printers aren't production-level printers. They're meant for creating prototypes when time isn't of the essence. It takes about four to five hours to print a mask and then about an hour to assemble everything.
Because of that time element, Yost is talking to manufacturers who could produce these in greater numbers. But the team is also openly releasing the plans so that anyone with a 3D printer can produce the masks.
In addition to creating the entire mask, makers could create just the disposable cartridge, which can be adapted to fit into the masks used in anesthesiology to deliver oxygen to patients.
TriEnda, Penda collaborate on urgent hospital bed shortage
Kruger Family Industries (KFI) has announced a critical collaboration between two key brands in their portfolio, TriEnda and Penda. These brands have joined forces to work to combat the severe and immediate need to address the upcoming hospital bed shortage related to the COVID-19 pandemic. The two companies will begin production of a newly developed product offering, a low-cost, and easily-assembled Emergency & Disaster Relief Bed.
The new Emergency & Disaster Relief Bed will be manufactured quickly in very large quantities. The beds are durable, easy-to-clean, and can be assembled on-site without tools in just a few minutes. Another feature of the bed is when they are no longer needed, they nest together efficiently for storage. The nesting allows for the reduced footprint of storage space and quick redeployment in future emergencies.
Penda is retooling a 300,000 square foot IATF 16949 certified automotive facility near Madison, WI to begin mass production of these hospital beds in the coming weeks.
Orders can be placed immediately for these beds, with production to begin early April and delivery to commence the week of April 13. More information about these beds can be obtained by contacting COVID-19@trienda.com, calling 608-742-8982.
Hy-Lite injection molding services available to support manufacturers
To help with the heightened demand for injection-molded products during the COVID-19 outbreak, Hy-Lite is making their contract injection molding services available to companies nationwide. Located in Pensacola, Fla., the Hy-Lite facility houses seven injection molding machines capable of small, specialty and slow run projects.
Steve Beck, plant/technical manager for Hy-Lite, a U.S. Block Windows Company, points out that, while Hy-Lite cannot manufacture safety masks or blow-molded items (such as hand sanitizer bottles), the company has many other options for supporting PPE needs.
Hy-Lite services are available on a contracted basis with speedy turnaround. Beck, who has been with Hy-Lite for more than two decades directing the company’s injection molding and manufacturing operations, explains that Hy-Lite can supply products made with most thermoplastics.
For more details on working with Hy-Lite Injection Molding Services, contact Steve Beck at 888.256.2599.
Roofing membrane manufacturer retools to manufacture PPE
Team members at Duro-Last Inc. – engineers, product development, and manufacturing staff – united to fabricate and manufacture isolation gowns and face masks. Using expertise in manufacturing flexible PVC and fabrics, the team went from prototype to production to delivery in one week.
The gowns are made from flexible PVC making them water and fluid-repellant. The masks are washable and reusable, made from polyester and PVC. Duro-Last reformulated products and retooled processes to manufacture these supplies.
Primex Plastics divisions join the COVID-19 fight
Primex Plastics Corp. has aggressively joined the fight against the COVID-19 virus by engaging its three divisions in producing vital materials for first responders and medical professionals. And all three divisions of the Primex One Company quickly responded.
In less than 24 hours, Primex Color, Compounding & Additives in Garfield, N.J. developed and started manufacturing a compound that is used to produce plastic vials for COVID-19 test kits.
Primex’s extrusion division is producing clear plastic sheet needed to manufacture face shields.
In just two days, in conjunction with Richmond’s Reid Health, Primex Design & Fabrication (PDF), designed and began producing replacement face shields for Reid’s bio helmets that protect clinical staff. In a press release Reid described PDF’s effort as an “Apollo 13 moment” where an unorthodox solution saved the moment.
PDF has also developed stand-alone shields, the PrimexProtect shield, and expects to go to production this week.
IgniteX COVID-19 Response Accelerator
From its prompting of citizens to socially distance themselves to its rising infection rates and economic devastation, the novel coronavirus pandemic has meant unprecedented, tragic disruption. It’s against that backdrop that a Black & Veatch initiative is leading a push to find and collaborate with startups and other innovators to expedite solutions that soften COVID-19’s impact on communities, with the hope that the future applications also extend beyond the pandemic itself.
As a virtual, remote effort, the “2020 Black & Veatch IgniteX COVID-19 Response Accelerator” is seeking emerging companies and entrepreneurs that have ideas about how to mitigate the coronavirus outbreak but who need help commercializing, rapidly deploying and scaling those concepts.
The range of possible solutions runs the gamut, from testing, screening and disinfection technologies to emergency medical facilities, autonomous delivery networks, biotech-related services, distance learning and training, and disease-tracking software.
Under the innovation-minded Growth Accelerator incubator within Black & Veatch – a global engineering, construction and consulting leader – the IgniteX COVID-19 Response Accelerator is committing at least $250,000 in grants or in-kind services. Those offerings will be used to support recruitment and collaboration as part of the campaign.
Cubic Partners, University of Alabama & prototype ventilator
Cubic Corporation has entered a partnership agreement with the University of Alabama in Huntsville (UAH) College of Nursing to use the Learning and Technology Resource Center’s (LTRC) Human Patient Simulator iStan to test an emergency ventilator device the company is developing in anticipation of ventilator shortages arising from the COVID-19 pandemic. Cubic’s Huntsville operations is the main development and manufacturing facility for its Cubic Mission Solutions business division’s GATR satellite communication and networking systems.
In collaboration with the staff at the College of Nursing’s LTRC, the GATR team used the iStan high-fidelity simulator (simulated patient) and reference ventilators to rapidly develop and test the emergency ventilator. The project, called VentiGATR, has now completed initial tests at the UAH College of Nursing and is in collaboration with Huntsville Veterinary Specialists and Emergency for live animal testing.
The GATR inflatable satellite antenna (ISA) is a lightweight, versatile satellite terminal extensively used across the Department of Defense to quickly establish communications for multi-domain operations for any mission, anywhere. The GATR team has repurposed off-the-shelf inflation components of the ISA to develop the compact VentiGATR prototype that is being used for testing.
Latest from Today's Medical Developments
- Exchangeable-head solid carbide cutting tools
- NextDent 300 MultiJet printer delivers a “Coming of Age for Digital Dentistry” at Evolution Dental Solutions
- Get recognized for bringing manufacturing back to North America
- Adaptive Coolant Flow improves energy efficiency
- VOLTAS opens coworking space for medical device manufacturers
- MEMS accelerometer for medical implants, wearables
- The compact, complex capabilities of photochemical etching
- Moticont introduces compact, linear voice coil motor