CREDIT: PEYTANT SOLUTIONS
Traditional implantable device materials – synthetic polymers, metals, and composite blends – often serve their mechanical purpose but may provoke a foreign body response. For example, stents used in interventional pulmonology to manage malignant airway obstructions can cause complications such as local inflammation and granuloma formation.
Another frequent problem from using these materials in the lung is the disruption of the body’s natural defenses. They can disrupt the mucociliary escalator that traps inhaled particles and germs in mucus, then propels the mucus and foreign material up and out of the respiratory tract using the beating of cilia. Disruption of a mucociliary escalator can lead to accumulation of foreign material and germs in the lung, including mucostasis and infection. The result can be frequent reintervention and/or the removal of the stent.
Now, a naturally occurring biologic material, human amnion, with a century of published medical use, is providing an alternative to these synthetic materials for medical devices. Peytant Solutions uses a component of human amnion – the amniotic membrane (AM) – to address some of the problems with airway stents. Working in collaboration with interventional pulmonologists and thoracic surgeons, Peytant has developed a human amnion-sourced biologic cover for use on pulmonary stents.
Peytant uses a proprietary process to decellularize human amnion, which is the inner lining of the placenta. The process removes all the cells and cellular components, while preserving the extracellular matrix (ECM). The result is an ECM membrane that can be used in place of the synthetic covers traditionally used on airway stents. Because this ECM membrane is similar to the ECM found throughout the body, it elicits little to no foreign body response.

Pre-clinical studies in a healthy porcine airway model showed the AM covering enabled the Peytant stent to integrate with native airway tissue as early as day 7 and achieve full integration by day 90. More importantly, the AM-covered stents demonstrated significantly less mucus build-up, no migration, less inflammation, and fewer obstructive granulomas, compared with a commercially available synthetic-covered control stent. The AM-covered stents also required no clinical interventions while the synthetic-covered control required periodic intervention and maintenance.
From a clinical translation perspective, this should mean the AM covering will allow the stent to be more accepted by the host. The objective is to reduce complications, improve luminal patency, and require less re-intervention – overall, improving patient quality of life.
Peytant’s new application for amnion is used in its AMStent Tracheobronchial Covered Stent System (AMStent System). According to its FDA de novo granted marketing authorization, the AMStent System is for use in the treatment of tracheobronchial strictures produced by malignant neoplasms in adult patients. These obstructions are common complications of lung cancers and metastatic tumors. An estimated 25% to 30% of patients with cancers in the lung will have pulmonary obstructions (PO). If untreated, POs can lead to life-threatening respiratory and cardiac failure.
The use of AM covers can replace synthetic covers that are the foundation of commercial stents today. Synthetic covers are frequently composed of chemicals such as expanded polytetrafluoroethylene (ePTFE) and thermoplastic polyurethanes (TPUs), forever chemicals which have raised growing health and environmental concerns. Reducing the use of these chemicals in medical devices would have the added benefit of protecting the environment and communities.

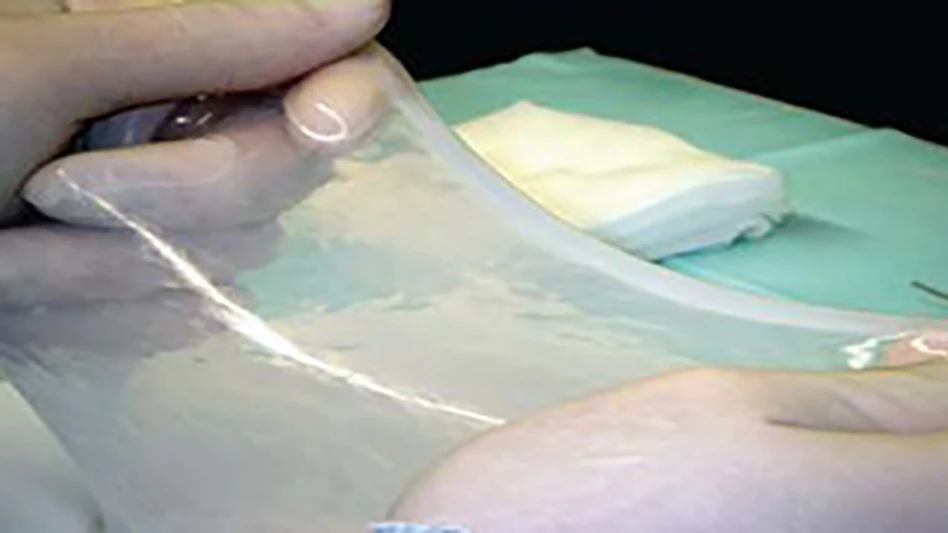
At Peytant’s manufacturing facility in Minnesota, the AM cover is attached to a self-expanding metal stent (SEMS) – an open cell nitinol stent scaffolding – so the stent is encapsulated in AM. The AM-covered stent is loaded onto a traditional over-the-wire deployment catheter for single-use application.
As the medical device industry shifts toward safer, smarter, and more sustainable solutions, the use of human-derived biomaterials such as amnion will continue to increase. The AMStent System not only sets a new standard for airway stenting but also opens the door for research into broader applications of amnion to devices used in multivascular, gastrointestinal, urologic, and gynecological procedures, all of which Peytant is exploring.
By leveraging a material the human body instinctively accepts, Peytant’s approach offers a glimpse into a future where implants are not just tolerated but welcomed into the body.
For engineers and clinicians alike, it is a powerful reminder that sometimes the best materials for treatment and healing come from the body itself.

About the author: F. Edwin Froelich, MD, JD, is medical director, Peytant Solutions. He bridges the complex intersection of healthcare delivery, innovation, and compliance, and contributes to the translation of novel therapies into practice while assuring patient safety and regulatory rigor. He serves as a liaison between clinicians, engineers, regulatory authorities, and corporate governance, ensuring that medical-innovation pathways are aligned with legal frameworks and patient-safety imperatives.
Latest from Today's Medical Developments
- Arterex unveils unified brand identity
- Dymax demonstrates light-curing material solutions for medical devices
- Able Medical Devices showcases latest sternal closure solutions
- TMTS 2026 explores AI-powered sustainable manufacturing and more
- QT9 QMS platform streamlines quality management, compliance for medical device manufacturers
- Spineology releases patient-specific expandable spinal implant
- Nordson EFD to demonstrate medical assembly automation applications
- Strategic partnership created to support early medical device innovation





