Photo by Chris Meyer, Indiana University
New technology developed by Indiana University Bloomington researchers could reduce the risks of treating heart disease – the No. 1 cause of death in Indiana – by improving the way surgeons restore blood flow to the heart.
IU’s Fibers and Additive Manufacturing Enabled Systems Lab is building microscopically thin fibers capable of sensing pressure in the veins. The FAMES Lab is working in partnership with Bloomington’s Cook Medical, the world’s largest privately owned medical device company, to improve tools such as endoscopes and catheters that doctors use to treat patients at risk for heart attack, as well as congenital heart defects, peripheral artery disease, and blood clots.

The development of these smart fibers also demonstrates IU’s important role in Indiana’s $99 billion life sciences economy, exemplified in part by the university’s newly signed Master Collaboration Agreement with Cook. This five-year agreement is expected to propel innovation through collaborations that foster innovation and support workforce development. It is also one of more than 450 active research projects across IU involving industry.
“The fiber offers a sixth sense inside the vein,” says Alexander Gumennik, director of the FAMES Lab, which is part of the IU Luddy School of Informatics, Computing and Engineering. “It can predict and prevent tissue damage critical to patient safety and assist the surgeon in the insertion of the medical device.”
Answering the call for solutions
“In meeting with Dr. Gumennik and his team, we recognized the versatility of the technology platform for clinical needs,” says Sean Chambers, director of research and development at Cook Medical. “The expertise and innovative approach that the FAMES Lab provided to this collaborative research project have been instrumental in advancing our understanding of the potential of fiber-based sensors in medicine.”
Equipping tools used to navigate the veins during minimally invasive medical procedures with smart fibers could revolutionize the treatment of heart disease. The smart fibers address a fundamental challenge of modern catheters: the lack of real-time sensory feedback as they pass through highly sensitive bodily tissues.
“It’s like trying to play guitar with only information from your eyes – no touch or sound,” Gumennik says.

of Informatics, Computing and Engineering | https://fames.indiana.edu/
Catheters are essentially thin tubes or wires with no feedback beyond what’s available from external imaging technologies like X-rays or MRIs. By contrast, the FAMES Lab sensors can provide immediate information from inside the body. A smart catheter that can sense pressure differences from being near a solid structure can tell whether it’s approaching a turn in the vein – or pushing dangerously against a vein wall – signaling to the surgeon to slow down or adjust course in real time.
The ability to sense this hydrostatic pressure – a sense unavailable to humans but common in animals such as fish – could also help medical professionals find the site of a blockage in the veins, ensuring the proper placement of interventional devices like stents.
More broadly, FAMES Lab’s groundbreaking sensors can also detect inputs like changes in temperature or acidity. Traditional sensors are significantly larger and harder – the smallest sensor chips are still about the size of a grain of rice and firm as rock – as opposed to fiber sensors, which are much safer for human tissues since they are elastic, flexible and as thin as hair.
Transforming invention into innovation
The innovation is powered by two core technologies developed at FAMES: a process for embedding micro- and nano-scale sensors and circuits into fiber, and another for controlling how materials heated to liquid form behave during fiber manufacturing.
“Think of it like a dripping faucet,” says Gumennik, who is also an associate professor of informatics at the IU Luddy School. “We can predict and control how the liquid core of the fiber breaks up and forms structures. This eliminates the need for trial and error and allows us to assemble functional devices inside the fiber itself.”
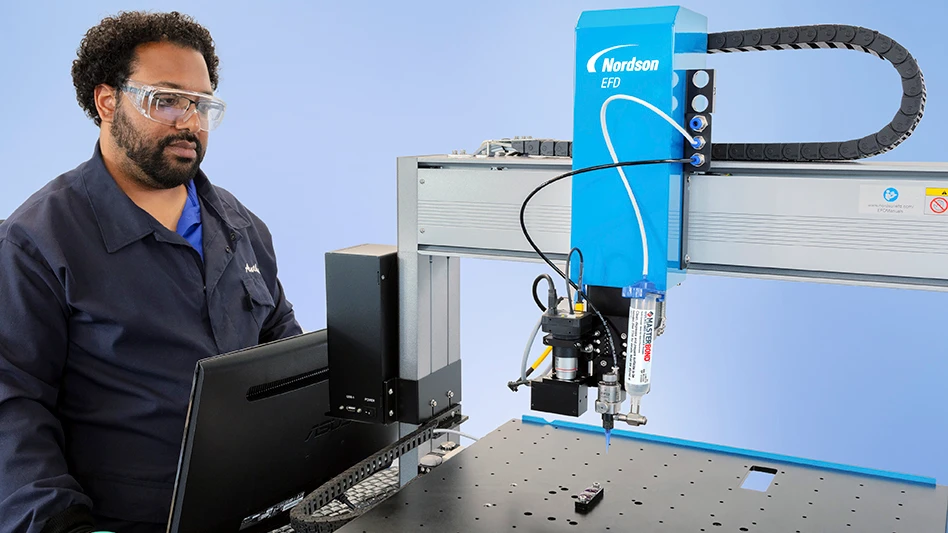
The centerpiece of IU’s FAMES Lab is a 27-foot tall, $1 million fiber draw tower – the source of the sensor production – surrounded by a 3,800-square-foot cleanroom. The state-of-the-art facility is uniquely designed to support industry-sponsored research projects, Gumennik notes.
Since joining Indiana University, Gumennik has disclosed nine inventions to the IU Innovation and Commercialization Office, resulting in at least seven patent filings and four granted patents with applications to fiber-based circuit integration, hydrostatic sensors and bioprinting.

In addition to smart sensors, FAMES Lab’s technology is also advancing research in areas such as quantum computing, communication and sensing, and biosynthetic tissue. One project in the lab – dubbed the cyborg flesh project – seeks to embed smart fibers into bio-printed material to create artificial veins to deliver nutrients and oxygen in the same manner as natural tissue. The long-term goal of that project is creating a “cardiac patch” to repair or replace damaged heart tissue.
Although the “smart catheter” technology developed under the Cook partnership has only been tested in simulated clinical environments, Gumennik says the technology is poised to advance toward the next steps in its path to the market.
As the first example of the type of innovations expected from IU’s new expanded relationship with Cook, Gumennik’s lab has forged a path for others across IU to now embark on.
“I really regard this project as the start of a long-term relationship,” he says. “Our agreement with Cook was not just beneficial to us; it also established a framework for future collaborations between Cook and IU.”
Latest from Today's Medical Developments
- Syringe-less injector system for diagnostic imaging obtains fourth FDA clearance
- Hohenstein Medical debuts enhanced medical device testing capabilities
- Arterex unveils unified brand identity
- Dymax demonstrates light-curing material solutions for medical devices
- Able Medical Devices showcases latest sternal closure solutions
- TMTS 2026 explores AI-powered sustainable manufacturing and more
- QT9 QMS platform streamlines quality management, compliance for medical device manufacturers
- Spineology releases patient-specific expandable spinal implant